Patients having threesomes, tranny Santa and Mrs. Claus stringing Christmas tree lights, doctors smuggling experimental drugs, Ed Koch dropping by -- all were part of St. Vincent's Hospital, the ground zero for AIDS and one time home to survivors of the Titanic, the Stonewall Riots, and 9-11. Four months out from the Catholic hospital's closing, Walter Armstrong compiled an oral history of the hospital's most harrowing and heartfelt moments from the peak of the epidemic to its final days.
Buried under a billion-dollar debt, St. Vincent's Hospital stands empty now, its last patient discharged April 30 as local residents rallied outside to protest the loss of a medical center that had served the West Village and Chelsea for 160 years. The ER, which had become a memorial site -- plastered with protest posters, letters of gratitude and grief, flowers and candles, even photographs of babies born in its delivery room -- is now boarded. At night, stripped of ambulances and sirens and flashing red lights, the city's last Catholic-run hospital takes on a ghostly aura as its bricks await the wrecking ball.
The closing of St. Vincent's has a special resonance for the generation or two of gay men who survived the AIDS crisis.
From 1981, when the hospital reported one of the very first cases of AIDS, to 1995, when HIV-related deaths peaked, St. Vincent's provided a setting for the desperate development of one of the nation's biggest and best HIV treatment centers. Driven by a sense of urgency that is now almost impossible to recapture, the gay community conspired with some remarkable doctors, nurses, and a nun or two to create an AIDS ward so unique -- and so different from the rest of the hospital -- that it seemed like another planet.
In the pause before St. Vincent's vanishes forever, Out asked me to collect the memories of some survivors of that time and record something of life on that planet. --Walter Armstrong
At ground zero of the epidemic, St. Vincent's had a mission to serve the gay men with ravaged immune systems and Kaposi's sarcoma lesions and rare infections who were showing up in the ER in ever-growing numbers. The quality of the Catholic hospital's mercy remains a contentious issue to this day.
Mark Chambers, Aids Ward Veteran
The early years are still like a horror movie that you have nightmares over, and then you realize it wasn't real, except it was. At St. Vincent's you didn't get inside the hospital -- you got into the emergency room, and that's where your friends were lined up on gurneys. My most vivid memory is of my best friend -- who I had gotten a call about 12 hours earlier -- still lying there, wasting and close to death, along with many other AIDS patients, waiting for attention. It was a scene of total helplessness on the part of both the patients and the staff.
Eric Sawyer, UNAIDS: The Joint United Nations Program On Hiv/Aids
When you call 911, the emergency ambulance takes you to the nearest hospital, so St. Vincent's was quickly overwhelmed. And even though they had some Catholic dogma-related policies that were homophobic, it was one of the few hospitals in the city that never turned its back on people with HIV.
Allen Roskoff, Gay Activist
Very early in the epidemic, Arthur Bell, the gay movie critic for The Village Voice, was in St. Vincent's, and he kept taking the crucifix off the wall, and the nuns kept putting it back up. Finally, he got so angry that he put the crucifix in his bedpan and pissed on it, and that caused a whole scene. After that, they were really nasty to him until [then-mayor] Ed Koch came to visit him.
Howard Grossman, Aids Doctor
I have a lot of respect for the people who did HIV work there, because they were not only fighting the epidemic, they had to fight the administration. The hospital was officially opposed to condom distribution, so people had to give them out secretly. That hypocrisy bugged the hell out of me, and I was relieved when I could admit my patients to other hospitals.
Joseph Sonnabend, AIDS Doctor
Until '85 or '86, they were not welcoming of this disease. The nurses were the compassionate ones. But I heard doctors making horrible jokes about gay guys. Some of my patients had dreadful experiences in the emergency room. Then things improved. Why? It may have been all the money in AIDS that became available. The hospital improved its PR--it put up billboards that said, we care. But nobody can say that all of a sudden St. Vincent's, institutionally, started to like gay people.
Barbara Starrett, AIDS Doctor
In 1982, the gay and lesbian doctors held a big meeting at St. Vincent's when Jim Curran came up from the Centers for Disease Control. He said very clearly what we all intuited--that AIDS was sexually transmitted and not easily communicable. Because of that, St. Vincent's always had open arms to anybody with HIV. In the beginning, there were aides afraid to come into a room, but thanks to the doctors and nurses constantly educating, that was soon not a problem. When I gave out condoms, the nurses would just look the other way.
The idea of a hospital floor devoted exclusively to AIDS was pioneered by San Francisco General's Ward 86 in 1983. In 1984, St. Vincent's followed suit, launching the nation's second AIDS ward. By 1986, one third of the hospital's 350 beds were filled by AIDS patients, and it was designated one of the city's first AIDS clinical care centers. In exchange for getting 30% higher reimbursement for each AIDS admission and other funding, St. Vincent's agreed to ramp up its services to people with HIV. In 1988, St. Vincent's started its Comprehensive HIV Center, for outpatient care and research -- in a ground-floor closet in a building across the street.
Lee Raden, AIDS Ward Resident Nurse
The hospital administration put the AIDS ward in Spellman, an old, dirty, nasty building. The rooms were small, single rooms that had to be made into doubles. It was hard to get beds and stretchers in and out. Spellman 7 was not a place that you would want to be -- with the spanking-new and shining Cronin building next door. But then we upsized: There were so many AIDS patients that they had to open up the Cronin side, because the seventh floors connected.
Some of the nurses were gay, but most were straight women with families, who had absolutely no experience with anything like this. Well, nobody had any experience with anything like this -- and yet they stepped up.
Maureen Satriano, AIDS Ward RN
Some nurses didn't want to rotate there because of homophobia or stigma, but most didn't want to because you had to work your ass off. AIDS is a multisystem disease, and you had to know about all the systems of the body. And no one was used to the sheer volume of meds that you had to give, not to mention the IV antibiotics for blood infections. We were also the only floor that had a lot of patients on ventilators, which is a lot of work--and we wanted to keep them on our floor because we didn't want anyone on the ICU messing up their treatment. It was the hardest I ever worked, but it was the best job I ever had. You were making a difference to someone every single minute of your shift.
Noel George, HIV Center research RN
Once you came into the ward, it was like you stepped into another place. There was warmth and love and compassion. The nun who ran the unit -- Sister Patricia -- was full of love. It was full all the time. Every day we admitted fevers, fevers, fevers. They were dehydrated; they had all these terrible infections. It was really kind of a hospice. But outside that unit, you were in trouble.
Lee Raden
I never thought it was a warm and fuzzy place. To have so many people a month dying on your unit was pretty much unheard of other than in a time of war. Anybody who walked on that unit knew how sick people were, knew that there was no cure, knew that there were no meds, and that the meds were killing people if the disease wasn't. I mean, I know I killed people with amphotericin B--but do you die from a fungal infection, or do you die from the drug? That's how it was in those days.
Most of the physicians, at the time, were young. Many were gay. They had come up with the epidemic, as we all did, and were also overwhelmed. They wanted to save the world and help patients with AIDS, but they were basically faced, from a medical perspective, with failure. We had doctors who flew in stuff from Mexico, only we couldn't administer it. So they sat by the bedside of patients and gave them all kinds of stuff that was not approved. It was unbelievable. In nursing, if you keep someone comfortable and allow them to die with dignity, you have a positive outcome. In medicine, death is never a positive outcome.
Barbara Starrett
I had a patient whose father was big in the Brazilian military. He flew to Paris and brought back HPA-23, the drug Rock Hudson was on, for his son. In the fall of '87, AZT became available, and my papers were in the mail the day it was released. As naive as I was, I was constantly thinking that a cure is just around the corner.
Another patient on Spellman 7 had KS in the lungs. He wasn't responding to chemo, and he did not want to die, but he was having respiratory problems, and he wanted to be intubated. He had no more lung tissue, and still I said, "You want to be intubated" -- he was turning blue -- "OK, you'll be intubated." Should I have said, in those last minutes, "Let me just hold your hand, and we'll let you go quietly. We'll give you a little morphine?"
Sean Strub, POZ Magazine Founder
Sometimes you would just drop by the AIDS unit with no specific person to see. You just made yourself useful. You knew where the clean linens were, you emptied urine bottles, and the staff was glad to have you around. I remember going in to see one guy, just a friend of a friend. He was too weak to speak -- just lifted up his hand, like he wanted me to touch it. And that was an odd feeling -- holding the hand of this person who was very, very ill and sitting there and understanding that I didn't have to say anything. Just being there for him to touch was as much as I could do.
But once I started going to ACT UP demos, I spent a lot less time at St. Vincent's.
Gay rage at the indifference of the government to the crisis in its midst took on muscular, media-smart form with the start of ACT UP in New York City's gay center -- conveniently located one block north of St. Vincent's. The hospital quickly became acquainted with both the hard edge and the soft side of its neighbor. And through the years, many members of ACT UP would spend their last days on the AIDS ward.
Gerri Wells, Activist
It was brought to an ACT UP meeting that a gay man was kicked out of the ER by a security guard because he had dared to kiss his lover. We all got to yelling and screaming in one of those heated conversations, and the whole room just got up, walked around the corner, and took over the waiting room in the ER. It really brought a lot of bad press: Here it was in the middle of Greenwich Village and gay lovers weren't considered family.
About five or six of us held meetings with the president of the hospital, the executive board, and a bunch of nuns. It took months to get the rule changed because Cardinal O'Connor lobbied against it. But we ended up getting all their employees to have sensitivity training.
Mark Aurigemma, former Gay Men's Health Crisis staffer
It was a very homophobic time because of AIDS. Public displays of affection that had started to catch on in the '70s had shut down completely. Touching or kissing your partner on the street was a very uncomfortable thing for many gay men to do. During the negotiations, we did a kiss-in -- a big demonstration of kissing that blocked 7th Avenue traffic in front of St. Vincent's for 45 minutes and allowed for a lot of pleasurable partner swapping. I think that was a real turning point at the hospital.
Gerri Wells
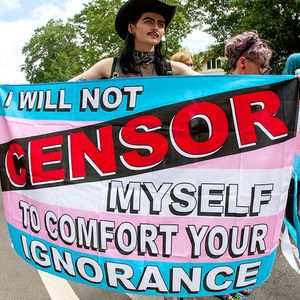
The ACT UP Christmas visits started because I had been going up to visit my brother on the AIDS ward and I saw that a lot of people had nobody, no family. I wore the Santa Claus outfit and Neil Broome wore the Mrs. Claus outfit and high heels. Rollerena would come in Rollerena drag. There were 10 or 15 people, and everybody wore different outfits. All the stores in the West Village would donate beautiful things as gifts.
So Neil and I would put on our little show: I'd knock him down on the ground and make everybody laugh. They liked it, unless they were very sick. Some would just give the look: "Leave something nice and get out of here, you wench. I know you're a girl under that beard. Get out!"
Sister Patricia, the nun who oversaw the unit, would quietly walk behind us. She said it was her favorite time of year, when we came.
Mark Aurigemma
The AIDS ward at St. Vincent's was a regular stop on many people's daily routine. Sometimes I would do multiple visits at once. I remember going to see Richard Dunne, the executive director of GMHC, who had kept his HIV secret for many years and when he got sick, he got PML [a brain infection] and declined very quickly. I also visited another friend down the hall named Montana Silkwood, a scrappy, lovely activist-restaurant worker-junk collector. Now Richard was a very regal person, and Montana was very, uh, eclectic, but I introduced them to each other, and they became friends up there. The AIDS ward was a great equalizer.
As the first drugs appeared and government funding increased, people with AIDS began counting their survival in years rather than months. But the death rate kept climbing on the AIDS ward (and in New York City) until July 1995, when the initial impact of combination therapy began bending the curve. By then, the AIDS ward had been open for a decade and had developed its own special rules, rituals, and rhythms. While life hardly moved to a disco beat, gay men had certainly succeeded in resizing the "sevens" to their own liberated dimensions. The unusually sensitive nursing staff understood that this is what an authentic community hospital at the intersection between the West Village and Chelsea, not to mention gay life and death, looked like.
Mark Chambers
My first time as a patient on the AIDS ward was in '98. I had a heart attack. I was 42. It had nothing to do with the condition of my heart and everything to do with protease inhibitors. And to tell you the truth, at first it was a little scary: I mean, the people there had AIDS -- imagine that!
The next summer, I developed very serious stomach problems. My doctor, Paul Bellman, sent me to the ER. They did a CAT scan, found an abscess in my intestine, and immediately did exploratory surgery. They wound up removing a foot of my small intestine because it was ulcerated, which they came back and told me was non-Hodgkin's lymphoma. I was told I had [the bacterial infection] MAI. I was told I had [the viral infection] CMV. They were giving me IV drugs that totally blew out my veins, so they put a Mediport in my chest--and within minutes, I've got a grapefruit-size bump on my chest. The nurse brings the surgeon, the surgeon brings the nurse. I'm off all my HIV meds because of the pending chemo. In the midst of all that, I still felt like they were taking care of me. I felt safe.
On my second visit, when I was there a lot longer, my boyfriend at the time helped make the room my own. And this was the case in a lot of people's rooms. They brought in all the memorabilia from home. All their own blankets, pillows, photographs, artwork, books -- whatever it took to make the person feel at home. And the staff supported that.
Sex was a little nerve-racking because you never knew who was going to walk through the door. The drill was we closed the door, pulled the curtain, and got on with it. One time my partner brought a third party along -- rather than bring flowers, you could bring a dick or an ass.
Lee Raden
All you could really do was help make whoever's life you came in touch with a little bit more comfortable. And if that involved their families, their friends, whatever, we tried to do it. We were writing it as we went along. And we made an awful lot of decisions autonomously, and we did things that were probably scandalous in other people's eyes.
We let patients smoke. We didn't have visiting hours. We let people spend the night in beds with their partner. We let people camp out in the rooms and on the floors and in the chairs for weeks at a time. There'd be people in drag. We would sneak people out on Gay Pride to go out to the parade: "Went down for a CAT scan," you know. There were even nurses who worked up there who were themselves trannies.
Maureen Satriano
If someone didn't have a healthcare proxy, and there was a disagreement between the lover and the mother, we knew that the lover had been there all the time and the mother had just arrived and was trying to take over. We wouldn't say it out loud, but we would sort of ignore the mom.
But sometimes the partner and the mom were best friends, and how nice was that for us, right? And we saw many people mend their relationships with families who may have ostracized them. Every family member who came to see a patient came to realize to some degree that this was not a gay man's disease and not a lifestyle choice -- that this was a human being with a terrible disease who needed to be taken care of.
Gene Fedorko
The day my lover, John, died, he was on a respirator. I knew it was time. I was his medical proxy, and he had always said that when it was time, to please stop the meds and the machines. The respirator was the only thing keeping him alive. But how was I going to remove the tube?
This guy was walking through the halls, his name was Richard--tall, longish blond hair, someone we knew from Provincetown but hadn't seen for 15 or 20 years. He saw me in the room and stuck his head in. I said, "What are you doing here?" He goes, "Oh, just visiting a friend." And he sized up the situation immediately. "I'm going to take the tube out of his mouth, OK?" And I said, "Please."
Somehow the AIDS ward being set up so that he could be walking through the hall--there was that kind of freedom--and just the coincidence of it all made hearing John take his last breath more bearable.
Maureen Satriano
We could usually tell within a few hours of when someone was about to die. Sometimes the patients told us. I'll never forget our first lesbian, and she was so angry, and she felt AIDS should never be happening to gay women. She came in with a throng of her friends, an entire entourage, who were just as angry as she was. She was released and stayed out of the hospital for a long time. But then she was diagnosed with breast cancer, and she was in and out of the ward until the end of her life. The friends got to know us and calmed down.
At the end, this woman who had been morbidly obese was down to 90 pounds and on a morphine drip. I went in to turn her and make her comfortable, and she said, "Can you close the door? I just want quiet to die by myself."
In 1996, the new class of protease drugs brought many AIDS patients back from the brink and freed most from their death sentence. St. Vincent's HIV clinic documented, for a leading medical journal, the complete reversal of the hospital's inpatient and outpatient trends from 1994 through 1996. Its AIDS ward, however, continued to meet a vital need long into its second decade as a more diverse, undiagnosed, and uninsured population filled its beds. But between the sensitivity trainings and the ghosts of all the beautiful boys that haunt it, the gay spirit hung around the hospital right to the end, by which point the weight of sin and scandal had largely shifted to the Catholic church -- and that other tribe of men in dresses.
Lee Raden
We had every kind of crazy queen and every color under the rainbow -- and some even I never imagined. I remember this one guy who was unbelievable. He was one of our frequent fliers and just way too sick. When the first protease inhibitor was still in trials, he got a doctor to put a stomach tube into his belly -- he couldn't keep anything down -- so that we could deliver it through a tube straight into his stomach. That's the lengths that this guy went through because he wanted to live.
And probably five years after I left St. Vinny's, this guy finds me at Rivington House, and he's on Rollerblades! We went out to lunch, and I'm like, "I can't believe you're alive," and the whole thing. And he said, "Do you remember the day you came into my room, and I wanted my doc to help me die, and you and Maureen talked me out of it?" And I was like, "I did?" And he's like, "Well, you didn't, but you did. You said..." and he remembered this clear as bells. I mean, we were in love with this guy, but it was probably just another crazy morning on the sevens, and he was on the bathroom floor, and we were like, "John, get up."
Mark Chambers
Even though I've left the Village and live in the country now, I can never see myself leaving Paul, my doctor. And similarly, I can never see myself being ill and not going to St. Vincent's.
The last time I was there, in 2007, the AIDS ward had gone from being an entire floor to being half a floor to being where now you don't know if the person in the next room has HIV or not. A lot of the gayness went. The special privileges were gone. There was a disconnect between nurses and patients. I missed the AIDS ward. I'd walk in and feel at home. There was a sense of aliveness about it, a sense of "Everybody's present and doing something about this." We were taking care of each other's IVs and meds and wiping each other's asses and doing whatever we could for each other. Today, if you do that, you've got two nurses telling you to get the hell away. It returned to normal. Isn't that sad?
St. Vincent's Timeline
1849
* In the midst of a cholera epidemic, St. Vincent's is founded by the Sisters of Charity, basically a poorhouse with 30 beds.
1861-65
* It provides care for veterans of the Civil War.
1912
* 106 survivors of the Titanic are taken from the Hudson River docks to St. Vincent's.
1969
* The first gay demonstration at the hospital is a candle-light vigil as Diego Vinales, fatally injured fleeing police during the Stonewall riots, is taken there in a coma.
1981
* St. Vincent's reports one of the nation's first 10 AIDS diagnoses.
* 214 diagnoses, 214 deaths*
1984
* Spellman 7 -- "the old building" -- is converted to an AIDS Ward, the city's first, with some 20 beds; it later expands to the seventh floor of the new building, Cronin, roughly doubling the number of available beds.
* 3,693 diagnoses, 1,973 deaths*
1985
* Community AIDS doctors smuggle experimental treatments into the U.S. and onto the ward for desperate patients.
* AIDS becomes the leading cause of death of men from New York in their 30s.
* 6,562 diagnoses, 3,797 deaths*
1987
* ACT UP is founded at the city's gay community center, around the corner from St. Vincent's.
* AZT, the first HIV drug, is approved. The dose, later viewed as toxic, was one capsule every four hours.
* 16,010 diagnoses, 9,859 deaths*
1988
* 22,447 diagnoses, 14,160 deaths*
1989
* Dr. Ramon "Gabriel" Torres is hired to head the HIV clinic. He aggressively pushes the hospital to conduct research, making it a leading site of clinical drug trials.
1992
* St. Vincent's cancels its World AIDS Day observance because the educational materials to be handed out promote condoms.
1995
* In June, the AIDS ward records its highest number of patient deaths in a single month.
* 93,825 diagnoses, 62,734 deaths*
1996
* Protease inhibitors, a new class of HIV drug, are released, restoring health to many people with HIV and turning AIDS into a chronic, manageable disease.
1997
* The number of AIDS deaths declines nationwide for the first time; in New York City, the drop is 50%.
* AIDS patients begin to be integrated into the general hospital population and the dedicated AIDS wards are closed one by one.
1998
* The hospital's refusal to approve a study of post-exposure prophylaxis following unsafe sex prompts Torres to leave. His 10-year legacy includes more than 40 clinical trials enrolling thousands of patients that earned the hospital hundreds of millions of dollars.
2000
* St. Vincent's merges with seven other failing Catholic-run city hospitals.
* 127,834 diagnoses, 80,489 deaths*
2001
* On 9/11, as the trauma center closest to Ground Zero, the hospital treats more than 800 survivors, with AIDS ward nurses recruited to the ER for their "war-medicine" experience.
2005
* St. Vincent's files for bankruptcy for the first time.
* 152,118 diagnoses, 92,627 deaths*
2008
* The hospital's in-patient admissions fall by 10%, with only 14% from the West Village and Chelsea
2009
* The hospital announces that it is filing for bankruptcy, with a $1 billion debt.
* The Pope warns against condom use, stating that they "increase" the "problem with AIDS."
2010
* After talks with six different city hospitals about possible partnerships founder, St. Vincent's files for bankruptcy
* April 6: The board announces it will close the hospital.
* April 9: The ER stops accepting ambulances.
* April 15: The last baby is delivered.
* April 19: More than 1,000 staff are laid off; a gay man with AIDS and longtime St. Vincent's patient is turned away from the ER.
* April 30: the ER locks its door, officially ending the hospital's 161-year run.
* The HIV clinic, under the leadership of Dr. Tony Urbina, continues to operate, under the auspices of the Center for Comprehensive Care at St. Luke's Roosevelt Hospital.
*New York City cumulative statistics
To view a slide show of St. Vincent's, click here.