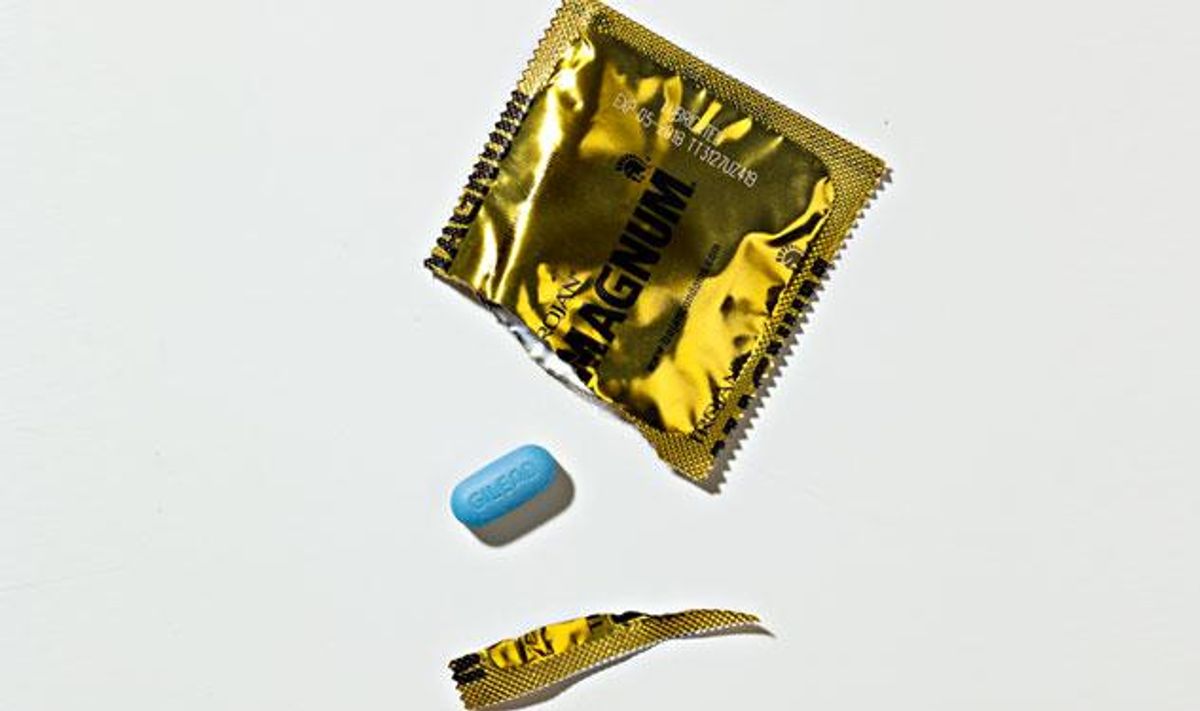
Taken once daily, the pill Truvada can prevent HIV. It’s safe, effective, FDA -approved, and usually covered by health plans. So why are so few gay men taking it?
September 09 2013 9:52 AM EST
December 05 2017 8:11 PM EST
By continuing to use our site, you agree to our Private Policy and Terms of Use.
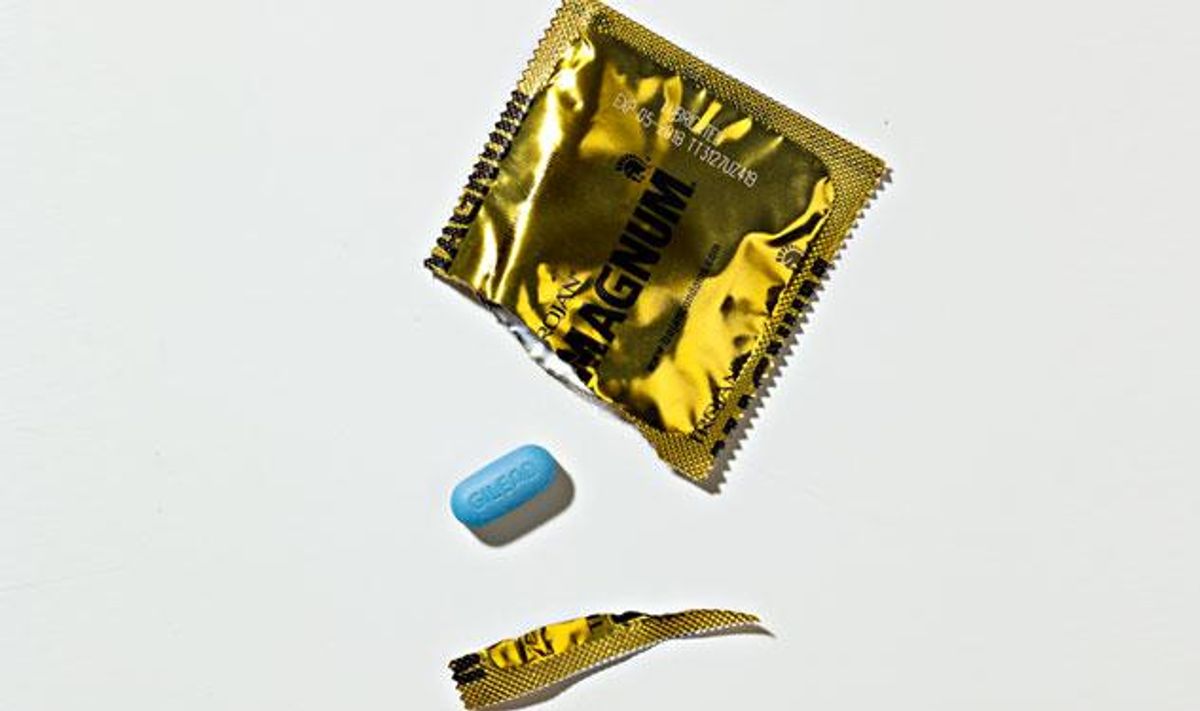
Taken once daily, the pill Truvada can prevent HIV. It’s safe, effective, FDA -approved, and usually covered by health plans. So why are so few gay men taking it?
Photography by Greg Broom
The gay 40-something well-known New York City doctor with many gay patients -- let's call him Dr. John -- can barely talk freely about what he's doing. "It's telling, how reluctant I am to talk about this, even anonymously," he says. "This isn't being talked about in our community at all."
The subject causing such anxiety for Dr. John is an oval blue pill called Truvada. He takes it once a day -- not to treat HIV, but to keep him from getting it. It's even covered by his insurance, thanks to a decision by the FDA last year to approve it as a prophylactic against HIV. That approval followed a groundbreaking study in 2010, called iPrEx, that found that HIV-negative gay men who faithfully adhered to a one-a-day regimen of Truvada reduced their risk of getting HIV by more than 99%.
Those findings, which HIV specialists had been keenly awaiting for several years, were enough to make Dr. John talk to his own doctor and start the regimen himself. "I don't want to become HIV-positive," he says. "But I don't love using condoms." Sexually active with multiple partners, Dr. John admits he avoided condoms about 20% of the time. He was tired of stressing constantly over whether he'd gotten HIV. "Even if my sex was relatively safe, I would have long periods where I'd be freaked out that something had happened."
Since he started taking daily Truvada, or PrEP (pre-exposure prophylaxis), as the regimen is called, Dr. John has remained HIV-negative and has experienced no side effects from the drug. "My sex life has been much less anxiety-provoking," he says. "Now if I don't use a condom, I feel like there's a safety net."
So why isn't he shouting about PrEP from the rooftops? Partly, he says, because he doesn't want people to think that because he's a doctor, he's endorsing PrEP for everyone: "There's a difference between giving medical advice and making individual choices."
But his reluctance is deeper than that. He also doesn't want to be judged for eschewing condoms from time to time. "Gay men talking about not using condoms is really stigmatized," he says. "Most of us have never known sex without condoms or without threat of a 'deadly disease.' " But he adds passionately, "I think it's a lot to ask an entire generation of gay men to use condoms forever."
Slow to Catch On
Dr. John is not alone in his reluctance to say that he doesn't always use condoms, or that he's on PrEP. I talked to dozens of LGBT health workers in the United States, as well as HIV-negative men on PrEP, and a clear picture emerged: Even though PrEP is the first proven new HIV prevention tool since the condom, and even though it's FDA-approved and is widely covered by health plans, few gay men appear to be on it.
"The uptake has been extraordinarily slow," says Dr. Bill Valenti, who works at an HIV-positive and LGBT-serving health care center in Rochester, N.Y. He says that of their 75 HIV-negative patients, three had started PrEP. At D.C.'s LGBT-serving Whitman-Walker Health, staff said that about 90 of their 3,000 HIV-negative patients had started PrEP. The clinic's patient population is made up primarily of African-American gay or bisexual men, the group at highest risk for HIV in the United States, along with transgender women.
It is difficult to know exactly how many guys in the U.S. are taking PrEP. Cara Miller, a rep for Gilead, the company that makes Truvada, said she couldn't pinpoint such numbers because the company doesn't know who is being prescribed Truvada in combination with other HIV drugs -- which is necessary for treating HIV -- and who is getting Truvada alone for PrEP purposes.
But Jim Pickett, who heads prevention advocacy at AIDS Foundation of Chicago, says that he has heard through inside sources that one of the country's largest insurers has, to date, covered only 300 prescriptions for Truvada alone, presumably for PrEP. That is a tiny number considering that Truvada, approved for use against HIV infection in 2004, has become a multibillion-dollar seller for Gilead. (The two drugs that comprise Truvada are sold separately or as part of the No. 1-selling HIV med, Atripla.)
Despite its slow uptake, PrEP comes along at a moment when it could potentially help reverse a 22% rise in HIV rates in young gay men in recent years, with young gay and bi men of color most affected. The CDC recently calculated that, if HIV infections continue to rise at current rates, half of young gay men will have HIV by age 50.
At the same time, the longstanding admonition to "use a condom every time," an approach pioneered in the '80s and '90s with posters and ads making condoms look sexy and fun, does not seem to be working. True, condoms are highly effective at protecting against HIV, as well as other STDs, including syphilis, herpes, and gonorrhea. They also sometimes break.
Moreover, studies since the 1980s have consistently shown that gay men forego condoms up to half the time, depending on the situation, for reasons ranging from "the heat of the moment" to alcohol and drug use to a plain old dislike of how condoms feel.
According to Pickett, this means that condom-only prevention campaigns will never succeed in bringing HIV rates close to zero. "If condoms were so wonderful and a part of human nature, we wouldn't have a problem with rising infections," he says.
And yet, PrEP doesn't seem to be catching on yet. Part of that is simply PR -- not enough people even know what it is. Miller says that Gilead prefers to support LGBT health centers in getting the word out over doing direct advertising. Why would they not go full throttle to boost sales of PrEP? "They know it would be a potential PR disaster," says Pickett.
And indeed, public reaction to PrEP has been mixed, with many concerned that widespread PrEP use will lead to an explosion of unprotected sex in gay men. Says Kevin Cates, who works in HIV prevention at Chicago's LGBT-serving Howard Brown clinic, "I hear a lot, 'Oh my God, this PrEP thing is so awful because people are going to bareback like crazy.' "
One group in particular, the large Los Angeles-based AIDS Healthcare Foundation, has taken a vocal stance against the FDA approval of PrEP, creating posters and other media warnings against it. Michael Weinstein, the group's president, says it's wrong for the FDA to have approved Truvada for PrEP when the iPrEx study showed that a large percentage of participants failed to take it once daily as prescribed. "It's giving people a false sense of security," he says.
Risks Involved
The truth is that PrEP comes with risks. Truvada can cause stomach upset in the first weeks of taking it. The drug, though low on side effects as HIV meds go, has been linked to mild kidney and bone problems in a small percentage of HIV-positive takers. However, Dr. Robert Grant, a professor at the University of California, San Francisco, and head of the iPrEx study, says he saw only mild side effects in his HIV-negative participants. Among the dozen or so men on PrEP with whom I spoke for this story, some of whom had taken PrEP for more than a year, none reported serious side effects.
It's true that if someone takes PrEP spottily, they lower the amount of the drug in their body, exposing themselves to HIV. There is also the possibility of developing resistance to Truvada, thus losing it as an HIV treatment option. Granted, Truvada is just one among many HIV treatment options. Moreover, Grant says that the only people in the iPrEx study who developed Truvada resistance were a few whose HIV infections were not picked up during the initial screening process.
The more you adhere to the recommended daily dosage of PrEP, the closer to 100% protection you get. According to Grant, those in the study whose blood levels indicated they used PrEP four times a week still had a 96% risk reduction. Those with blood levels showing they used PrEP twice a week had 76% risk reduction. Grant says that experts still aren't certain exactly how little, and at what intervals, one can use PrEP to have it still be effective, which is why one pill daily is currently recommended.
There is also validity to fears about "barebacking." Even if PrEP protects against HIV, condomless sex still invites other STDs. Some, like syphilis, gonorrhea, and herpes, are fairly easily treatable. But in recent years, there have been outbreaks among HIV-positive men of sexually transmitted hepatitis C, for which treatment is improving but still difficult, expensive, and imperfect. In certain parts of the world, such as Japan and India, a new antibiotic-resistant strain of gonorrhea has rung alarm bells of a new STD epidemic. Simply put, nobody knows what new infections lie in wait down the road.
But despite those risks, several PrEP users I spoke with said they were unfazed. "I'm not going to let fear rule my life," says Damon Jacobs, 42, a Brooklyn family counselor who has not only taken PrEP for two years now, he's also started a Facebook page, "PrEP Facts: Rethinking HIV Prevention and Sex," to promote an open conversation and breaking news about it. Dr. John admitted he worried about getting hep C or drug-resistant gonorrhea, but "so far, I haven't gotten any STDs, so it's an abstract concern."
"I have to admit that since being on PrEP, I've become much riskier," says "James," 51, a New York City computer programmer.
Importantly, recent research has made it clear that HIV-positive people reduce their chance of passing on the virus by 96% if they take meds that make their blood levels of HIV consistently undetectable on tests.
James says he began PrEP because he has multiple sex partners and hates condoms -- "Every instinct in my body says I don't want to wear them" -- but he didn't want to potentially pass HIV to his HIV-negative boyfriend. "I can't tell him I'm on PrEP, but I'm trying to protect him," he says. He's contracted chlamydia a few times, he says, but in the near year he's been on PrEP, he's stayed HIV-negative.
PrEP As a Health Booster
Then again, there is the argument that being on PrEP actually makes people safer because it raises their consciousness about their health. The iPrEX study found that participants reported decreased anal sex and increased condom use, though that might partly be because participants were regularly meeting counselors as a requirement of the study. In addition, participants initially did not know whether they were on Truvada or a placebo.
Being on PrEP requires seeing a doctor four times a year for an HIV test and kidney and bone tests. Being that connected to one's health, say PrEP advocates, may actually bolster safer choices.
That seems to be the case for Gustavo Varela, 25, a program coordinator for an LGBT youth group in Chicago. Varela was on PrEP in the iPrEx study, but isn't on it currently. "I used condoms when I was on PrEP, and if I went back on PrEP, I would still use condoms," he says. So why be on PrEP at all? "I've had slip-ups where I didn't use a condom in the heat of the moment, or if I was drinking," he admits. "It's an extra precaution."
That extra protection is also sought by Darius Mooring, 34, an African-American college bookstore manager in Bethlehem, Penn. He says he is researching if his health plan will cover PrEP. "There are times I use condoms and times I don't," he says. "I will have sex with guys who I know are HIV-positive."
"If I go on PrEP, will I be condomless in all my sexual encounters?" Mooring asks. "I don't think so. But I'm not going to live in fairy tale where I tell myself I use condoms all the time. PrEP will be adding another strategy to my HIV prevention."
That is how PrEP advocates want to frame it -- as another tool in the kit of HIV prevention, in the mix with condoms, monogamy, negotiated safety, and keeping HIV-positive people treated and undetectable. For example, you might be on PrEP and forego condoms with your HIV-negative boyfriend, but use them when you play outside the relationship. Or you may go on PrEP for periods of time when you're having multiple partners, then off PrEP once you're in a relationship.
Daring to Talk About It
Certainly, PrEP may be a good option for guys who put themselves at risk again and again. At D.C.'s Whitman-Walker Health, Dr. Raymond Martins speaks of a patient who came to him three times for post-exposure prophylaxis, or PEP, otherwise known as the HIV "morning-after" regimen: After possible exposure to HIV, a patient takes HIV meds for a month to block the infection.
According to Martins, that patient is a perfect candidate for PrEP. "He never uses condoms. Better that he's on PrEP as a permanent backup for his lifestyle than come in every month for PEP."
In some ways, it's easy to accept PrEP if you think of it as an extreme solution for turbo-sluts who fail again and again to use a condom -- if, in other words, you pathologize it. Several friends I spoke with about this story said they couldn't understand a person having such a hard time using condoms that they would have to actually go on an HIV med to prevent getting HIV. To that, PrEP advocates say it's far safer to be on Truvada for a period of time than to live with HIV for a lifetime. Even well-treated HIV has been shown to have myriad effects on health, such as accelerated aging, in the long-term.
But it also can be easy for us to forget that only 30 years ago, nobody thought of a condom as a routine part of sex. "If HIV infections truly were a hetero issue, there'd be an alternative to condoms by now," says Dr. John. "I don't think the world of straight men would settle for using a condom their whole lives."
Several men I talked to for this story told me of their dislike of condoms defiantly, without shame. In Boston, hairstylist Scott Owen, 48, said he'd never used condoms and had somehow stayed HIV-negative all these years. "I don't like condoms," he says. "I can't enjoy sex with them. They desensitive it for me. I always just figured that if I became HIV-positive, I'd deal with it."
When he heard about the Boston branch of the iPrEx study four years ago, he immediately signed up. He's off PrEP now that he's finished the study, but he wants to go back on it. He also wants to do another upcoming study, to test the effectiveness of a rectal microbicide gel.
That gel may be among the many new tools in the HIV prevention arsenal years down the line. Others in development include looking at another HIV drug, Selzentry, for use as PrEP, as well as "mini-vaccines" that would require injections three or four times a year. Meanwhile, studies of Truvada as PrEP continue as a way to assess effectiveness, adherence, and safety over time.
Advocates often talk of PrEP in birth-control terms: If a condom is like a diaphragm, then PrEP is the Pill, with perhaps more options in the works. "Women change methods of contraception over time," says Pickett. Likewise, he says, "No one thinks of PrEP as a lifetime strategy. It's for when you need the support."
In the meantime, Dr. John has no apologies for being on PrEP, even if he's not ready to go public about it. "We need to be able to talk about our desire to have sex without a barrier," he says. "Sex is about getting as close to someone as you possibly can. I think we're entitled to that. And as long as the answer is, 'Well, you should just wear a condom all the time,' you're obviously not reaching everybody."
Want more breaking equality news & trending entertainment stories?
Check out our NEW 24/7 streaming service: the Advocate Channel!
Download the Advocate Channel App for your mobile phone and your favorite streaming device!